The purpose of Men’s Health Week is to raise awareness of preventable health problems and encourage early diagnosis and treatment of diseases among men and boys.
Men’s health in the UK is unacceptably poor. Men will die 4.5 years earlier than women on average, for largely preventable reasons, and one in every five men will die before reaching the ‘traditional’ retirement age of 65. Cancer, suicide, and heart disease are the main causes of death among men of working age.
According to a recent survey, men are reluctant to speak with their GP, with 23% entirely refusing to seek medical advice on health issues due to embarrassment.
The survey asked men why they put off visiting their GP and the reasons given were:
- Too busy to go (29%)
- Worried about burdening the NHS (28%)
- Unable to get an appointment around work hours (26%)
- Embarrassment or awkwardness (23%)
- Worried about catching germs (22%)
Encouraging men to seek help is vital to them regaining control of their health and enjoying longer and healthier lives. We’ll delve into men’s mental health, prostate, and testicular cancer, and where they can find help and guidance.
Mental health
Mental health stigma has typically been a huge barrier as to why men have not traditionally seeked help, not wanting to be deemed weak or incompetent, feeling ashamed and embarrassed that they need support with their mental health.
UK data on men’s mental health is concerning, and more effort still needs to be done to encourage men to seek help.
- Three times as many men as women die by suicide – suicide is the biggest cause of death in men under the age of 50
- Men aged 40-49 have the highest suicide rates in the UK
- 73% of adults who go ‘missing’ are men
- Men are three times more likely than women to become alcohol dependent
- Men are more likely to use (and die from) illegal drugs
Even though mental health issues can affect anybody, regardless of age, gender, ethnicity, or social status, society has historically made it easier for women to talk about and express their feelings than it has for men. This is due in part to traditional gender roles and society’s expectations of men, as well as the associated shame or stigma men might feel if they decide to seek help.
It’s good to talk!
Reaching out and talking to someone you trust is the first step in the right direction in getting the care and support you need. You should also contact your GP who can discuss how you are feeling and then they can help advise on the best ‘next steps’ for you. There are many treatments for depression and by talking to your GP they can help signpost you to the right support and treatments, for example, talking therapies, referring you to a mental health specialist, such as a psychiatrist, counselling, local support options or medication.
Mental health resources for men
The websites listed below are excellent sources of knowledge, with many of them targeted exclusively to men and their issues.
- ManHealth
- ManUp? (mental health charity)
- Mental Health Foundation
- Heads Together (works to reduce the stigma around men’s mental health)
- Movember (looking at mental health through a male lens)
- The Samaritans
Prostate cancer
Prostate cancer is the most common cancer in men across the UK with more than 47,700 men diagnosed with prostate cancer every year. This means that 1 in 8 men will get prostate cancer in their lifetime. Men with prostate cancer often have no symptoms unless the disease is detected at a late stage.
Common prostate cancer symptoms that can also be caused by an enlarged prostate include:
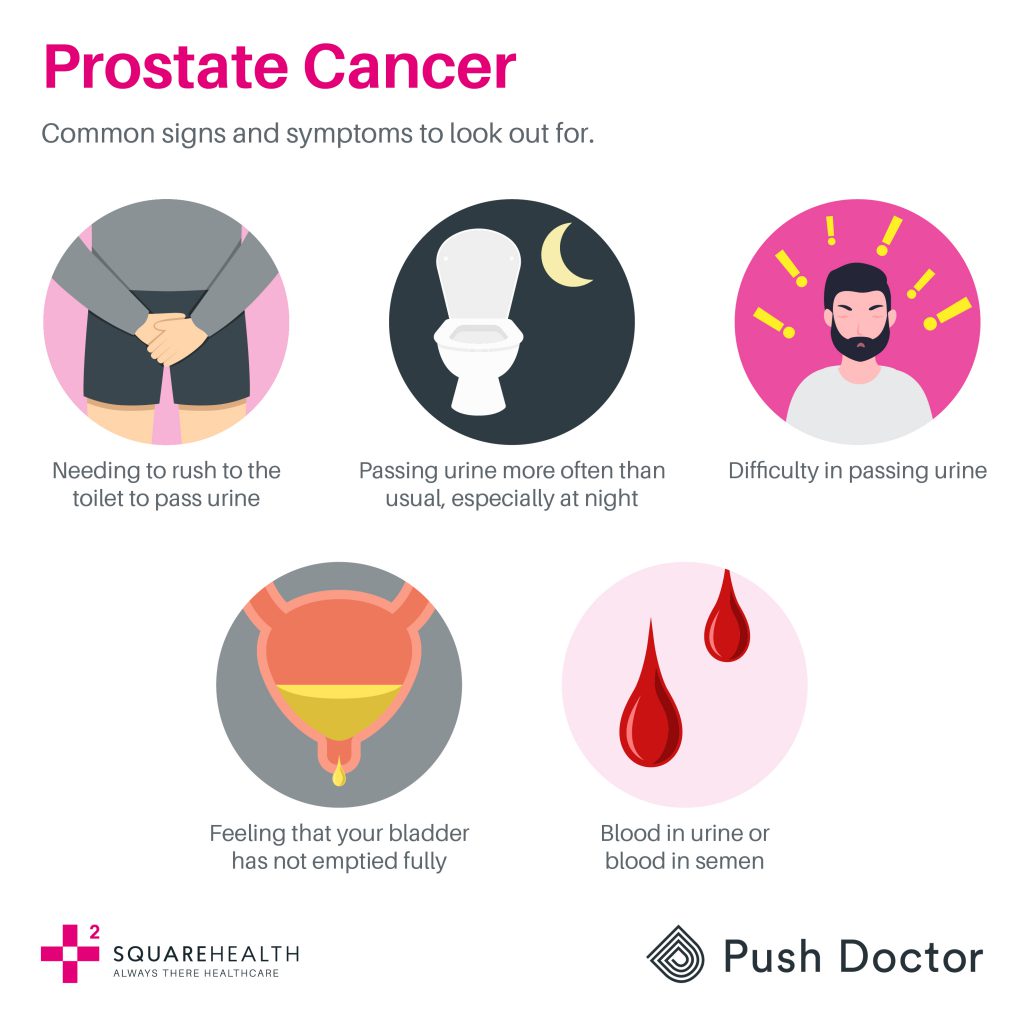
However, it’s still important to see your doctor and get checked if you experience any changes or symptoms.
Nearly half of all men are expected to develop prostate cancer at some point in their life. The chances of survival are extremely high in those that are diagnosed when there are no symptoms and when the disease is confined to the prostate gland.
Black African or African-Caribbean men are more likely to get prostate cancer than other men. The reason for this is unknown, although it might be linked to genetics.
There is currently no national NHS screening programme for prostate cancer, although men aged 50+ can speak to their GP to see if they are eligible for PSA testing, so screening is vital in protecting your health and early detection of prostate cancer could save your life!
For more information on prostate cancer visit Prostate Cancer UK.
Testicular cancer – it’s time to check your balls!
Testicular cancer is a relatively rare type of cancer accounting for 1% of all new cancer cases in males. However, it is the most common cancer in men aged 15-49 years in the UK, with testicular cancer rates peaking in the 30-34 age group. Testicular cancer for reasons that are unclear is more common in White males, than Asian or Black males.
Like many cancers, the incidence of testicular cancer has risen significantly since the 1990s and twice as many British men are now getting the disease as they did in the mid-1970s.
There are no known preventable risk factors that have been identified that increase the risk of testicular cancer and as a result, it is not possible to prevent testicular cancer. However, several factors have been identified that could increase your risk of developing the disease and these are:
- Undescended testicle(s) as a baby
- Family history – having a close family member who had testicular cancer or an undescended testicle(s) as a baby can increase your risk
- Previous testicular cancer – men who have been previously diagnosed with testicular cancer are between 12 and 18 times more likely to develop it in the other testicle
The good news is that following diagnosis and treatment of testicular cancer, long-term survival is excellent with 10-year survival rates of 98%, so early detection is key.
Self-examination is a simple and entirely safe method of detecting changes in your testicles. It is important to do this regularly to be aware of your ‘normal’ testicles and therefore to detect changes at an early stage.
Testicular Cancer UK has a great video that shows you how to check your balls, take a look here.
Encourage your father, brother, partner, husband, cousin, or friend to be upfront about their health and, when symptoms arise emerge, to seek medical help rather than delaying or putting it off.





