Cervical Screening Awareness Week happens every June to promote awareness about the importance of cervical screening. Attending your local doctor’s practice for a routine screening test is not something we look forward to, but it is vital to get examined because there are 3,200 new cases of cervical cancer diagnosed in the UK each year, which equates to approximately nine diagnoses each day. The good news is that 99.7% cases of cervical cancer are preventable.
In this article, we will look at the anatomy of the cervix and understand how an infection from certain types of human papillomavirus (HPV) causes nearly all cervical cancers. HPV will also be discussed, as well as the common symptoms of cervical cancer and how to reduce your risk along with discussing screening.
The cervix
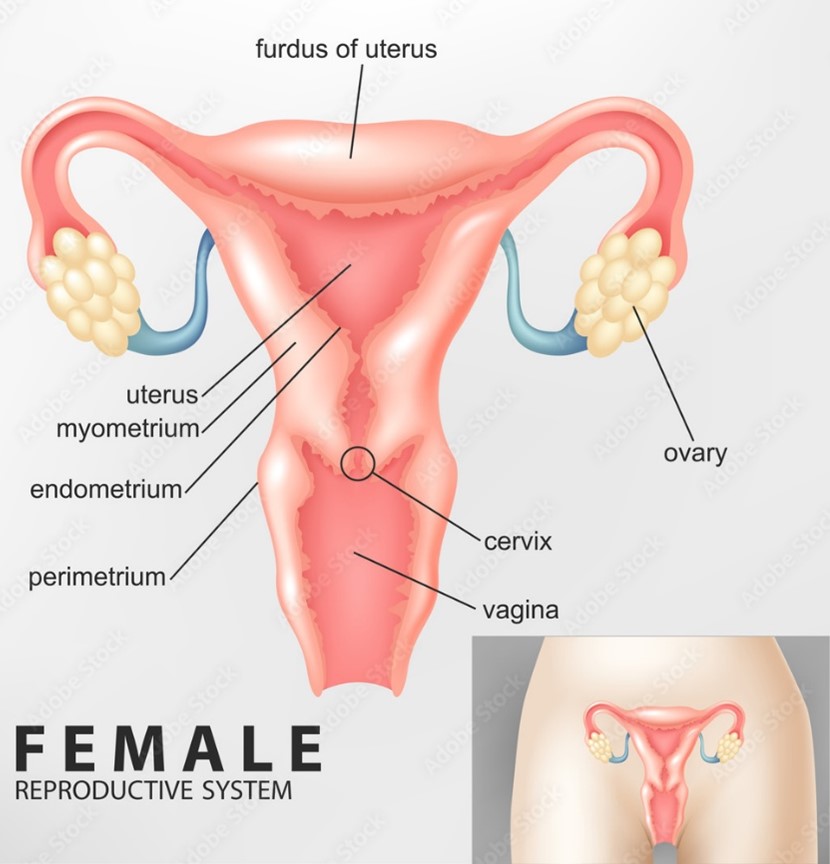
The womb and the cervix are both parts of the female reproductive system, with the cervix being a strong muscle that serves as the opening to the vagina from the womb (see image below).
What is the transformation zone?
The transformation zone is the location where cervical cells are most likely to become cancerous. It is the area just around the opening of the cervix that leads onto the endocervical canal (the narrow passageway that extends up from the cervix into the womb). During a cervical screening, the doctor or nurse will examine the transformation zone. Cervical screening is not a cancer test. It is a screening test that looks for abnormal cervical cells and if these abnormal cells are not treated, they may develop into cancer.
What is HPV?
Human papillomavirus (HPV) is a virus that affects both men and women. 90% of people are exposed to when they become sexually active. In most cases, the virus clears with no harmful consequences, but in a small percentage of women, it causes pre-cancerous and potentially cancerous changes to the cervix. There are many different forms of HPV, but the high-risk strains (particularly numbers 16 and 18) are more typically connected with cervical problems.
Cervical screening looks for high-risk types of HPV and if present, the sample is then checked to see if there are any changes in the cells so treatment can be provided before the cells have a chance to become cancerous. Boys and girls are now given the HPV vaccine starting at the age of 12. This means that with a combination of HPV vaccine and regular cervical HPV screening, cervical cancer is close to 100% preventable.
What are the symptoms of cervical cancer?
When it comes to cervical cancer signs and symptoms, you should know what to look for. If you are suffering any of the symptoms listed below, you should see your GP as soon as possible and get yourself checked out.
- Unusual bleeding (such as: between periods, during or after sex, or after the menopause)
- Pain and discomfort during sex
- Unpleasant smelling vaginal discharge
- Persistent pelvic and/or back pain
- Weight loss

How to reduce your risk
There are also several lifestyle changes that can significantly reduce your risk of cervical cancer including:
- Reporting any abnormal bleeding/symptoms to your GP
- Getting vaccinated against HPV (Human papillomavirus) if you are in the correct age group
- Having regular cervical screening appointments from the age 25+
- Stopping smoking – find out more about starting an NHS smoking cessation programme
Cervical cancer screening (smear tests)
Attending a cervical smear test can seem intimidating and cause anxiety for several reasons – including not knowing what to expect, embarrassment, and fear of an uncomfortable experience. Whilst these are valid concerns, cervical smear testing is often quick and painless and some of these tips can help make the experience more comfortable.
Being invited for a smear test
All women and people between the ages of 25 and 64 who have a cervix should have regular cervical screening. You will receive a letter in the post inviting you to schedule an appointment (make sure you are registered with your local GP surgery).
The NHS cervical screening in England is shown below:
| Age | When you’re invited |
| Under 25 | Up to 6 months before you turn 25 |
| 25 to 49 | Every 3 years |
| 50 – 64 | Every 5 years |
| 65 or older | Only if one of your last three tests was abnormal |
Visit the NHS cervical screening page here for more information.
Having a smear after the menopause
After going through menopause, some women find the smear test more painful. But why is this the case? Following menopause, oestrogen levels fall, causing the vaginal skin to become less elastic. As a result, the speculum device used to open the vagina is often more painful. This can be remedied by using HRT, either topically applied oestrogen cream into the vagina or as part of traditional HRT.
Self-sampling for HPV – the way forward for screening
To combat declining smear test attendance rates among women, the NHS started a trial of self-sampling (at-home) HPV kits in London. The NHS is hoping that the ‘YouScreen’ trial will remove any barriers for women to get screened because they can do it in the privacy of their own home (it’s similar to inserting a tampon). If the trial is deemed successful, self-sampling could be offered to women as part of the national screening plan as an alternative to traditional smears.
You can order self-sampling HPV kits privately from a variety of local pharmacy suppliers.
So please don’t be afraid of the smear and make sure you get screened, it could save your life.





